Breakthrough Cures for Hepatitis C Still Fail to Reach the Vast Majority of Americans Who Need Them
A new CDC report suggests the majority of people with hepatitis C still have not been cured1 nearly a decade after breakthrough treatments that clear the viral infection were first approved in the United States. The findings highlight the urgent need for a proposed national program that would end much of the suffering and death from hepatitis C by eliminating the disease in the United States.
It’s estimated more than 2 million people in the United States have hepatitis C, which if left untreated, often leads to serious and sometimes deadly outcomes such as liver cancer and liver failure. Despite the existence of a safe and highly effective oral cure for hepatitis C, the infection contributed to the deaths of more than 14,800 people in 2020.
“Tens of thousands of Americans with hepatitis C are getting liver cancer, suffering liver failure, or dying because they can’t access lifesaving medicine,” said Jonathan Mermin, M.D., M.P.H., Director of CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention. “In our nation, no one should have to live knowing a cure for their potentially deadly disease is available, but out of reach.”
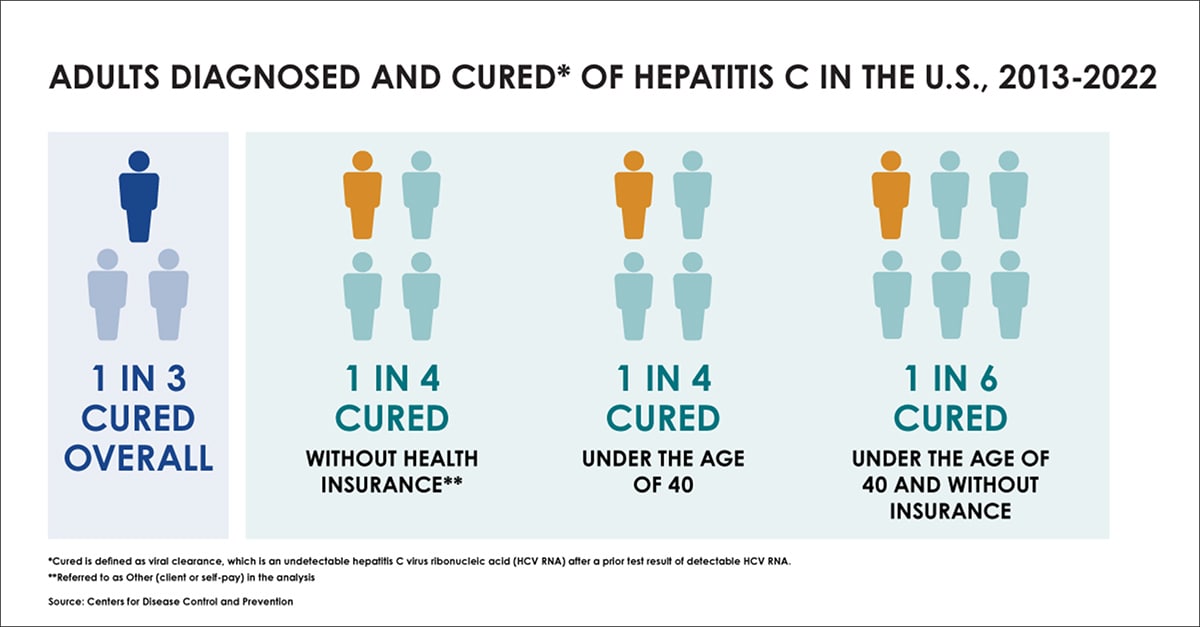
The new CDC study indicates jarringly low numbers of people with known hepatitis C virus infection are being cured and provides the first clear picture of the small proportion of people without health insurance who have been cured. The data indicate the proportions of people cured were:
- Low overall and across all age and insurance groups analyzed
- Lowest among people without health insurance2 or with Medicaid coverage, as well as adults under the age of 40 – a group that has the highest rates of new hepatitis C infections
- Highest among people 60 and older with Medicare or commercial insurance, yet still less than half had been cured
Barriers & Solutions to Hepatitis C treatment
“The development of a safe and highly effective cure for hepatitis C is one of the most stunning medical achievements of the past 20 years,” said Francis S. Collins, M.D., Ph.D., of the National Institutes of Health, who serves as the lead of the White House National Hepatitis C Elimination Program. “But unfortunately, too many people in our country still face insurmountable barriers to accessing this treatment – which means we must work harder. The proposed National Hepatitis C Elimination Program includes bold and transformative actions that will overcome many of these barriers, potentially saving tens of thousands of lives and tens of billions of health care dollars – compassionate care that also contributes to deficit reduction. This is a truly historic opportunity.”
Current barriers to hepatitis C treatment include (but are not limited to):
- Cost of treatment
- Restrictive treatment coverage policies
- Challenges diagnosing hepatitis C
Cost of treatment: Although the cost of hepatitis C treatment has decreased during the past decade, it is still a barrier for many, with medication that costs tens of thousands of dollars. An innovative national hepatitis C drug delivery model would make treatment attainable for everyone, including people who are under- and un-insured.
The White House has requested substantial funding needed across federal agencies to enact this and other key steps to reach hepatitis C elimination in the United States. Such investments will ultimately save billions in healthcare spending within ten years, and prevent tens of thousands of cases of cirrhosis, end-stage liver disease, liver cancer; and save thousands of lives.
Restrictive treatment coverage policies: Some state Medicaid programs and commercial insurance providers still have treatment restrictions in place. These often include restrictions that:
- conflict with medical guidance
- limit which patients are eligible for treatment (for example: requiring patients to have severe liver damage or go months without using alcohol or drugs before treatment)
- limit what types of providers can prescribe treatment
- require prior authorization before treatment can begin
Policymakers and insurers should consider removing treatment coverage restrictions that make it difficult or impossible for people with public or private insurance to access treatment to cure hepatitis C.
Challenges diagnosing hepatitis C: Testing for hepatitis C in the United States requires an antibody test, and if that is positive, a lab-based nucleic acid test to confirm infection. This process is cumbersome, results in some people never getting a confirmed diagnosis, and delays treatment.
Additional resources could be used to support the development and approval of rapid point-of-care (POC) viral tests for hepatitis C, which would allow people to be tested and connected to treatment in a single visit. Such tests, along with an adequately funded comprehensive public health effort to expand prevention, testing, and treatment to more settings, is vital to:
- Diagnosing the 40% of people with hepatitis C in the United States who are unaware of their infection
- Expanding access to prevention services to curb new hepatitis C infections
Federal experts and scientists believe that despite these barriers, the United States can still seize the opportunity to become a world leader in preventing suffering and death from hepatitis C. Achieving this goal will require commitment in the forms of increased resources, policy change, and dedication to the idea that all people with hepatitis C should benefit from the game-changing cures for hepatitis C – today, not in another ten years.
1 Cured is defined as viral clearance, which is an undetectable hepatitis C virus ribonucleic acid (HCV RNA) after a prior test result of detectable HCV RNA
2 Referred to as Other (Client or Self-Pay) in the analysis