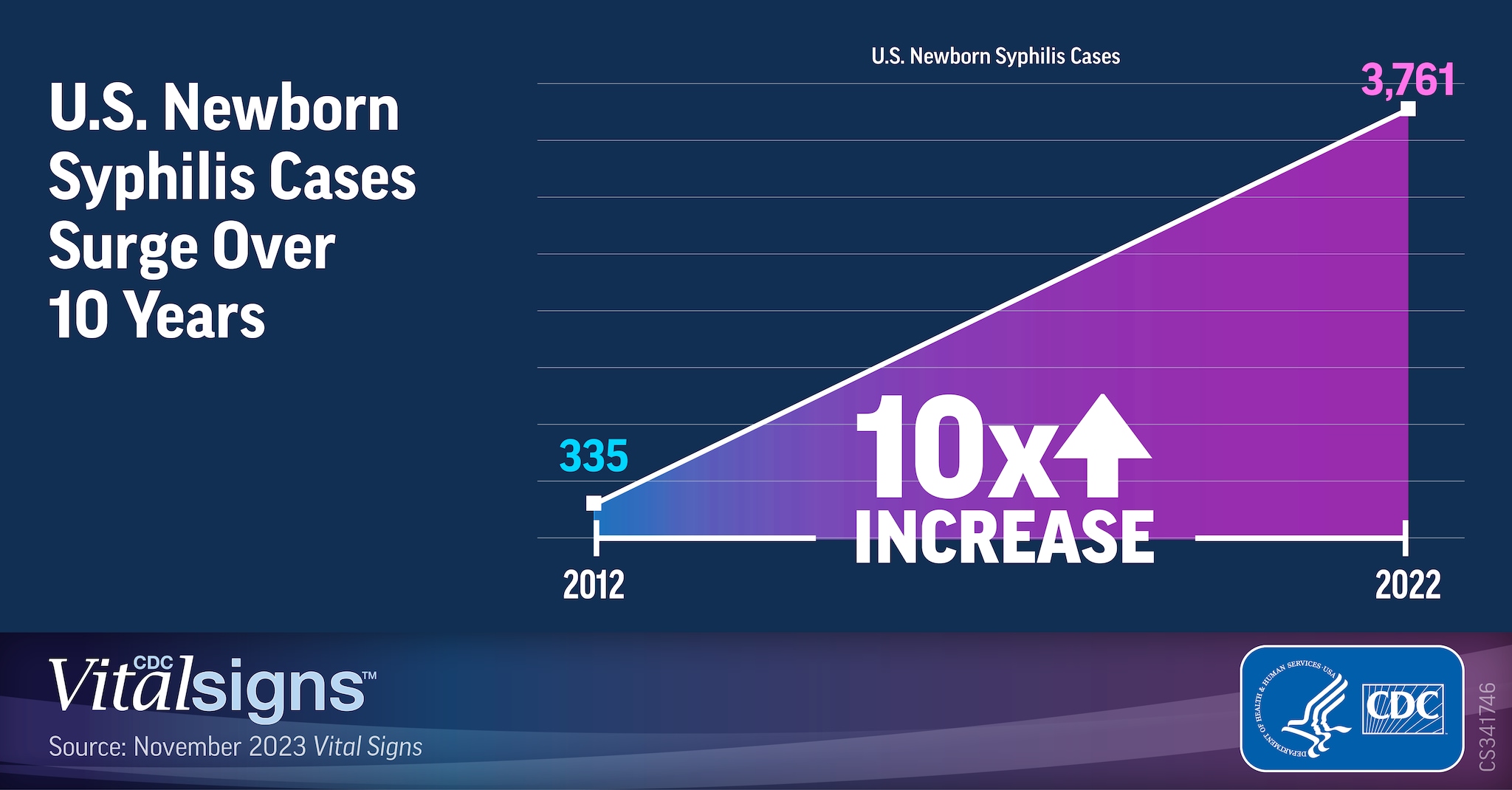
U.S. Syphilis Cases in Newborns Continue to Increase: A 10-Times Increase Over a Decade
CDC is recommending concerted action to stop the increase of newborn syphilis cases and continues to sound the alarm about the consequences of a rapidly accelerating epidemic of sexually transmitted infections in the United States. Syphilis during pregnancy can cause tragic outcomes, like miscarriage, stillbirth, infant death, and lifelong medical issues. Newborn syphilis occurs when mothers do not receive timely testing and treatment during pregnancy.
New CDC data reveal that more than 3,700 babies were born with syphilis in 2022, which was more than 10 times the number in 2012. The increase in newborn syphilis follows rising syphilis cases among women of reproductive age combined with social and economic factors that create barriers to high-quality prenatal care and ongoing declines in the prevention infrastructure and resources.
“The congenital syphilis crisis in the United States has skyrocketed at a heartbreaking rate,” said CDC Chief Medical Officer Debra Houry, M.D., M.P.H. “New actions are needed to prevent more family tragedies. We’re calling on healthcare providers, public health systems, and communities to take additional steps to connect mothers and babies with the care they need.”
Key findings
- Almost 9 in 10 cases of newborn syphilis in 2022 might have been prevented with timely testing and treatment during pregnancy.
-
- More than half were among people who tested positive for syphilis during pregnancy but did not receive adequate or timely treatment.
- Nearly 40 percent were among mothers who were not in prenatal care.
One of the biggest risk factors for syphilis for some people is where they live. According to previous CDC data, in 2021, more than 70 percent of the U.S. population lived in counties considered to have high rates of syphilis among reproductive-age women (above the Healthy People 2030 target).
Barriers to timely syphilis testing and treatment during pregnancy
Missed opportunities to prevent newborn syphilis during pregnancy are due to a combination of individual and system-level barriers to timely syphilis testing and treatment. Individual-level barriers may include lack of insurance and substance use disorder, while system-level barriers may include systemic racism and limited healthcare access.
Tailored prevention strategies are critical to addressing newborn syphilis disparities
People from racial and ethnic minority groups are experiencing the brunt of the newborn syphilis epidemic. While newborn syphilis cases are increasing overall, babies born to Black, Hispanic, or American Indian/Alaska Native mothers were up to 8 times more likely to have newborn syphilis in 2021 than babies born to White mothers. Such disparities stem from decades of deeply entrenched social determinants of health that create greater obstacles to quality healthcare services and result in health inequities such as higher rates of syphilis in some communities. Community health workers, including local patient navigators, case managers, and disease intervention specialists, are critical components to developing tailored strategies to reduce newborn syphilis in every community. They play one of the most powerful roles in addressing racial and ethnic disparities in congenital syphilis.
“The congenital syphilis epidemic is an unacceptable American crisis. All pregnant mothers—regardless of who they are or where they live—deserve access to care that protects them and their babies from preventable disease,” said Jonathan Mermin, M.D., M.P.H., director of CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention. “Our nation should be proactive and think beyond the OB/GYN’s office and bridge prevention gaps. Every encounter a healthcare provider has with a patient during pregnancy is an opportunity to prevent congenital syphilis.”
CDC is urgently encouraging public health leaders and any healthcare provider with pregnant or reproductive-age patients to:
- Consider starting syphilis treatment right away following a positive rapid syphilis test during pregnancy if the patient faces greater obstacles to ongoing care (and still send for full confirmatory syphilis testing for optimal patient follow-up).
- Use rapid syphilis testing and treatment during pregnancy in settings such as emergency departments, syringe service programs, prisons/jails, maternal and child health programs.
- Address syphilis before pregnancy in counties with high syphilis rates, by offering to screen sexually active women and their partners for syphilis, as well as people with other risk factors for syphilis.
- Work with local community health workers who can help to overcome additional barriers to syphilis testing and treatment during pregnancy.
Due to the increase in cases of syphilis and congenital syphilis in the United States, senior leadership at the U.S. Department of Health and Human Services (HHS) established the National Syphilis and Congenital Syphilis Syndemic Federal Taskforce dedicated to spearheading a national syphilis and congenital syphilis public health response. The overarching mission of this task force is to address the syndemic of syphilis and congenital syphilis, reduce their rates, promote health equity, and share resources with impacted communities.
For more information about this report, go to www.cdc.gov/vitalsigns.